Understanding cancer requires understanding that tumors are not isolated masses of malignant cells.
In Episode 57 (https://www.linkedin.com/posts/activity-7393693938945273856-tZHm?utm_source=share&utm_medium=member_desktop&rcm=ACoAAC7R33oBU_8RoYPHRDoVcF5C0OEYKzEXkxY), we explored why CAR-T therapies fail in solid tumors, highlighting physical, metabolic, and immunosuppressive barriers. Today, we map the cellular and molecular architecture of the TME:
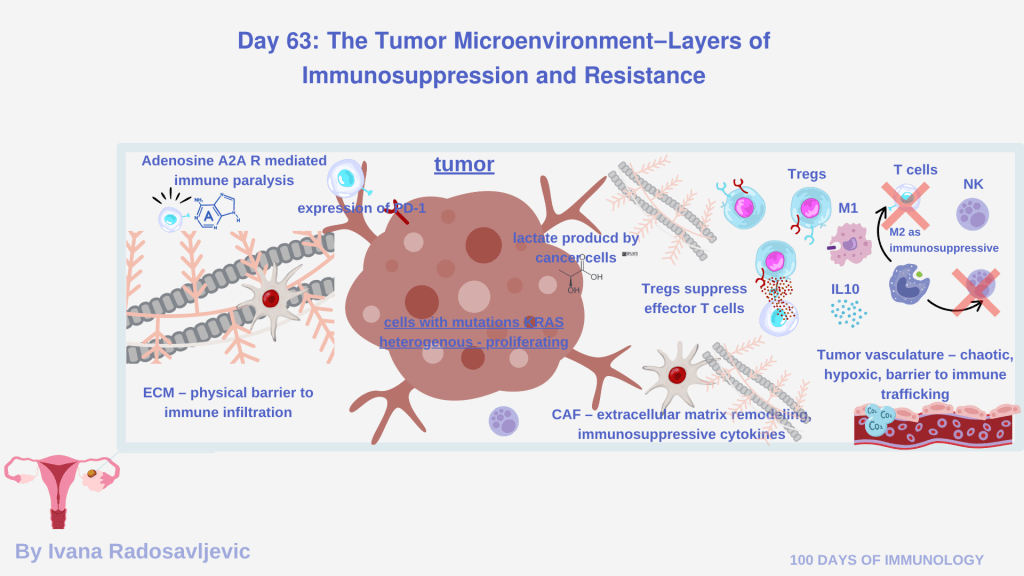
𝟭. 𝗖𝗲𝗹𝗹𝘂𝗹𝗮𝗿 𝗔𝗿𝗰𝗵𝗶𝘁𝗲𝗰𝘁𝘂𝗿𝗲 𝗼𝗳 𝘁𝗵𝗲 𝗧𝗠𝗘
• Tregs (FOXP3⁺) – suppress via IL-10, TGF-β, and IL-2 depletion [1]
• TAMs (M2-like) – pro-angiogenic, ECM-remodeling, IL-10⁺, Arg1⁺ [2]
• MDSCs – inhibit via ROS, NO, and amino acid depletion [3]
• Exhausted CD8⁺ T cells – PD-1⁺, TIM-3⁺, LAG-3⁺ profiles [4]
• Dysfunctional DCs – impaired priming of effector T cells
• Cancer-associated fibroblasts (CAFs) – produce collagen, CXCL12 barriers
• Endothelial cells – create abnormal vasculature and hypoxia
• Tumor cells – express PD-L1, CD47, produce lactate
𝟮. 𝗣𝗵𝘆𝘀𝗶𝗰𝗮𝗹 𝗕𝗮𝗿𝗿𝗶𝗲𝗿𝘀
• Dense extracellular matrix (collagen I/III, fibronectin)
• High interstitial pressure
• Hypoxic regions
• Abnormal vasculature – reduces immune cell infiltration
𝟯. 𝗠𝗲𝘁𝗮𝗯𝗼𝗹𝗶𝗰 𝗕𝗮𝗿𝗿𝗶𝗲𝗿𝘀
• Hypoxia → HIF-1α induction + VEGF secretion [5]
• Lactate accumulation → T cell dysfunction
• Adenosine (CD39/CD73) → A2A-mediated immune paralysis
• IDO–kynurenine pathway → Treg expansion and NK suppression
𝟰. 𝗦𝗼𝗹𝘂𝗯𝗹𝗲 𝗮𝗻𝗱 𝗠𝗼𝗹𝗲𝗰𝘂𝗹𝗮𝗿 𝗜𝗺𝗺𝘂𝗻𝗼𝘀𝘂𝗽𝗽𝗿𝗲𝘀𝘀𝗶𝘃𝗲 𝗙𝗮𝗰𝘁𝗼𝗿𝘀
Cytokines: IL-10, TGF-β, IL-6
Checkpoint signaling: PD-1, CTLA-4, TIM-3
Chemokines: CXCL12–CXCR4 barrier
CD47–SIRPα (´don’t-eat-me signal´)
Antigen loss, MHC-I downregulation, and APM defects
𝟱. 𝗚𝗲𝗿𝗺𝗮𝗻 𝗥𝗲𝘀𝗲𝗮𝗿𝗰𝗵 𝗟𝗲𝗮𝗱𝗲𝗿𝘀
Prof. Dr. Peter Friedl (University of Tübingen) – cell-tumor interactions, therapy resistance
Dr. Bettina Weigelin (University of Tübingen) – Mechanisms of immunotherapy, TME imaging, resistance
Prof. Dr. Eran Elinav (DKFZ) – Cancer microbiome, host-microbiome-TME interactions
𝗤𝘂𝗲𝘀𝘁𝗶𝗼𝗻 𝗳𝗼𝗿 𝘁𝗵𝗲 𝗔𝘂𝗱𝗶𝗲𝗻𝗰𝗲: If you could remove one suppressive component from the TME which would you target first?
Stay tuned for 𝗗𝗮𝘆 𝟲𝟰: 𝗡𝗲𝗼𝗮𝗻𝘁𝗶𝗴𝗲𝗻 𝗩𝗮𝗰𝗰𝗶𝗻𝗲𝘀 – 𝗣𝗲𝗿𝘀𝗼𝗻𝗮𝗹𝗶𝘇𝗲𝗱 𝗜𝗺𝗺𝘂𝗻𝗼𝘁𝗵𝗲𝗿𝗮𝗽𝘆
𝗥𝗲𝗳𝗲𝗿𝗲𝗻𝗰𝗲𝘀
1. DOI: 10.1084/jem.20210831
2. DOI: 10.1016/j.celrep.2017.12.011
3. DOI: 10.1158/2326-6066.CIR-16-0297
4. DOI: 10.1038/nri3862
5. DOI: 10.1038/nrc3726
#Immunology #TME #TumourMicroenvironment #SolidTumors #Immunotherapy #OncologyResearch #100DaysofImmunology #CellTherapy #TMEBarriers #CancerResearch #GermanyScience #ImmunoOncology